Complications After Breast Augmentation: What You Need to Know
| ABCS
Breast augmentation is a cosmetic procedure that increases the breasts’ size and enhances their shape, usually with the placement of silicone gel- or saline-filled breast implants beneath the chest tissues. While this is one of the most popular cosmetic surgeries, it is also a serious surgical procedure that is not without risks.
Understanding the details of breast implant surgery is important to making an informed decision, so here, we describe the potential complications, how fat transfer may offer an alternative to breast implants, and steps toward making an informed decision.
Breast augmentation complications:
- Capsular contracture
- Rippling
- Implant displacement
- Risks associated with the surgery
- Breast implant rupture
- Additional surgeries (breast implant revision or removal surgery)
- Systemic symptoms (Breast implant illness, BII)
- Effects on breastfeeding
- Anaplastic large cell lymphoma (BIA-ALCL)
- Changes in sensation
- Poor scar formation
Capsular contracture
Capsular contracture occurs when the scar tissue that naturally forms around the implant tightens abnormally and compresses the implant. This tightening causes the breast to feel hard and appear warped or high on the chest. Capsular contracture cases range from mild to severe, and are classified using a scale called the “Baker grades” which range from I to IV. Grade I may not require treatment, while most patients want to address Grade III or IV.
It is one of the most common complications of breast implants, occurring in about 10% of patients. It is thought to be related to a bacterial biofilm that can form around the breast implant, and thus surgeons try to minimize implant handling and potential bacterial contamination with techniques such as using a Keller Funnel. They may also avoid periareolar incision placement (around the nipple-areola complex) and subglandular placement (above the chest muscle), as these techniques are also associated with a higher capsular contracture risk.
If a patient develops capsular contracture, a breast implant revision surgery may be required to remove the hardened scar tissue capsule. Patients may choose to have their implants removed or to replace the implant, which involves a risk of capsular contracture recurrence.
Rippling
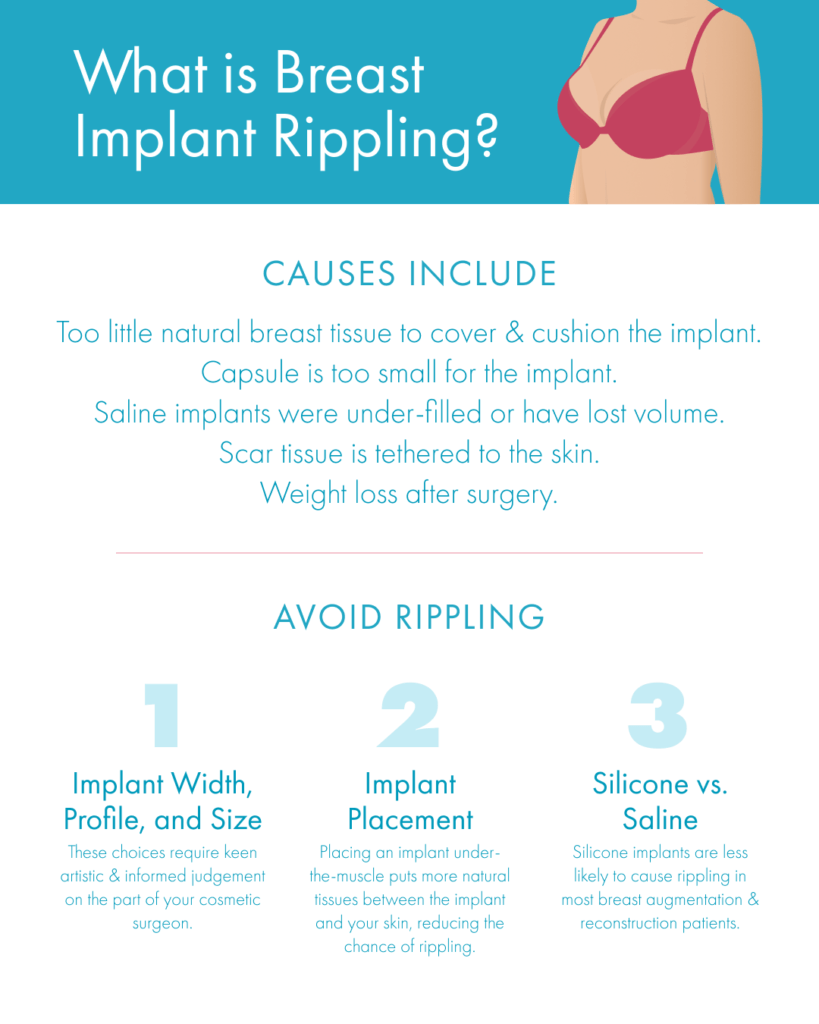
Rippling refers to wrinkling of the implant which is visible through the skin. While this poses no health risk, this is considered to be a cosmetic complication.
Rippling can occur with both saline and silicone implants, but is more common with saline. This phenomenon is more likely in women with thin natural breast tissue, and can be minimized by placing the implant beneath the chest muscle and choosing an appropriately sized implant for your frame and tissues.
If you have very little natural breast tissue, your surgeon should talk with you ahead of time about their plan for breast implant sizing and placement to help you achieve the most cosmetically sound outcome possible.
Implant displacement
Sometimes, implants may be improperly placed by an inexperienced surgeon, or move from their original positioning over time, leading to asymmetry or an unnatural appearance. This is called implant malposition or implant displacement. Corrective surgery may be necessary to reposition or replace the implants.
Implant displacement is uncommon in the hands of a breast surgery expert, as creating the correctly sized breast implant pocket and choosing an appropriately sized implant will help to prevent this. Be sure to carefully vet your surgeon by looking at reviews, before and after photos, and their training specifically in cosmetic breast surgery (more information on choosing a surgeon below).
Risks associated with the surgery
Bleeding, infection, reactions to anesthesia, hematoma, and seroma are all risks in the period of time immediately following surgery. Your surgeon should screen you for any risk factors beforehand and provide thorough aftercare instructions to help prevent these complications. If you have worsening or persistent symptoms after surgery, it is critical to communicate these with your cosmetic surgeon so that you can promptly treat any problems.
Breast implant rupture
The outer silicone breast implant shell, whether it is filled with sterile saline or with cohesive silicone gel, can rupture. If an implant ruptures, revision breast surgery should be performed to remove or replace ruptured implants, as implants are designed to be safe inside the body when fully intact.
Saline implant ruptures are noticeable immediately: the implant will deflate and the saline inside will be safely absorbed by the body. But, because the filling of modern silicone implants is cohesive and does not tend to migrate, silicone breast implant ruptures usually require an MRI or ultrasound scan to detect; these are known as “silent ruptures.” The FDA recommends that patients with silicone implants undergo a scan at intervals after having had their breast implants for 5-6 years.

Additional surgeries (breast implant revision or removal surgery)
While this is not technically considered a complication, most patients who have breast implants will have another surgery to replace or remove their implants at some time in the future. Undergoing breast augmentation means that you should expect additional surgeries over time.
It is normal and safe to seek out revision surgery both to change the cosmetic appearance of the breasts or to treat a complication. And, it may comfort you to hear that, while breast implant warranties last about 10 years, it is not necessary to replace your implants after a specific period of time if you have no complications and are happy with your breast appearance; many patients keep their implants for 20 years or longer without any issues.
Systemic symptoms (Breast implant illness, BII)
Breast implant illness or BII is a term used by many people to describe systemic symptoms that are thought to stem from breast implants (either saline or silicone). Reported symptoms resemble those of autoimmune conditions, and may include fatigue, joint or muscle pain, hair loss, brain fog, or respiratory issues.
BII is not yet a specific, official medical diagnosis because research into this nuanced pattern of symptoms is still ongoing. While many patients have seen symptoms resolve after removing their breast implants with an explant surgery (breast implant removal), symptom resolution is not guaranteed. The current research supports screening breast implant patients who have systemic symptoms for autoimmune conditions to rule those possible issues out before proceeding with plans for implant removal.
Effects on breastfeeding
Most women are able to successfully breastfeed with breast implants. But depending on the details of your surgical plan, including where your surgeon places your incisions, breast augmentation surgery may impact your ability to breastfeed in the future. If you hope to breastfeed after surgery, ask your surgeon to discuss the details of their surgical techniques and whether or not this could affect you.
Anaplastic large cell lymphoma (BIA-ALCL)
Though extremely rare, there have been reported cases of anaplastic large cell lymphoma, a type of non-Hodgkin’s lymphoma, associated primarily with past styles of breast implants that have a highly textured surface. BIA-ALCL is not a form of breast cancer, but rather a cancer of the immune system. Due to increased understanding of BIA-ALCL, cosmetic surgeons typically now use breast implants with a smooth surface.
BIA-ALCL typically presents as either a mass in the breast or an unexplained swelling or delayed seroma occuring many years after the initial placement of the implants. With early detection, BIA-ALCL may be treatable with breast implant removal and capsulectomy (removing the breast implant capsule).
Changes in sensation
Nipple and breast sensitivity can increase or decrease after breast augmentation, and it is possible to have some pain associated with breast augmentation. While these changes are usually temporary, in rare cases, they may be permanent.
Poor scar formation
We have many advanced techniques to help scars heal with a flat appearance and very close to the patient’s natural skin color. However, sun exposure can darken scars; straining incisions during the healing process may lead to more noticeable scars; and sometimes, for no known reason, a patient’s scar may become raised or appear darker than their skin tone.
To prevent visible scarring, follow your surgeon’s aftercare guidelines, protecting your incisions and taking care to avoid becoming too active before you are fully healed and given the go-ahead. Many surgeons recommend silicone gel or silicone strips once your incision is closed to help minimize scars. If you are still unhappy with your scar’s appearance, treatments available to help fade scars include steroid injections, topical microneedling, and laser treatments.

Making an informed decision
Fat transfer as a breast implant alternative
Fat transfer breast augmentation, or fat grafting, is an alternative to breast implants for patients looking for a small increase in breast size—up to about 1 cup size, or 200 ccs of volume. This involves a first step, liposuction, to harvest fat from areas where you have available or extra fat, such as the thighs, abdomen, or flanks. Then, your own harvested fat is purified and carefully reinjected into your breasts to improve asymmetry, add cleavage, and/or increase volume.
Fat transfer does not carry a risk of capsular contracture or systemic symptoms, but this is still a serious surgical procedure that involves potential risks and complications of its own. Further, there is a risk that some of the fat (estimates vary, but about 25-50%) will fail to “take” in the breasts and will be reabsorbed by the body in the months following surgery. Experienced cosmetic surgeons will account for this likelihood in their surgical plan; a secondary fat transfer procedure may be needed to achieve your desired results.
Questions to ask your cosmetic surgeon
A trustworthy surgeon will go over all of the potential complications with you in a thorough consultation, answering patient questions such as:
- What are the most common complications you encounter? The most common complication of breast implants is capsular contracture, so a surgeon having uncommonly high rates of other complications is a red flag.
- How do you minimize the risk of complications? Techniques like the Keller Funnel for placing breast implants with zero direct handling can help to minimize risks of infection and capsular contracture. Most surgeons also avoid textured-surface implants in favor of smooth-surfaced breast implants.
- Where do you operate? Surgeons should operate only in accredited private surgical facilities or hospitals that are monitored for staff training, sterility, and equipment needed to handle complications or emergencies. Our guide to facility accreditation »
- What is the plan if a complication does occur? Your surgeon should talk with you about how they handle possible complications so you are aware of the full extent of the risks and potential associated costs.
Every surgery carries risks, and it is important to weigh these against the possible benefits. Being well-informed and choosing a board-certified cosmetic surgeon can significantly reduce your risk of complications.
References »
Risks and Complications of Breast Implants. 12/15/2023. U.S. Food & Drug Administration.
Questions and Answers about Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). 10/23/2019. U.S. Food & Drug Administration.
FDA Strengthens Safety Requirements and Updates Study Results for Breast Implants. 10/28/2021. U.S. Food & Drug Administration.
Larsen A, Rasmussen LE, Rasmussen LF, Weltz TK, Hemmingsen MN, Poulsen SS, Jacobsen JCB, Vester-Glowinski P, Herly M. Histological Analyses of Capsular Contracture and Associated Risk Factors: A Systematic Review. Aesthetic Plastic Surgery. 2021 Dec;45(6):2714-2728. doi: 10.1007/s00266-021-02473-3.
Swezey E, Shikhman R, Moufarrege R. Breast Implant Rupture. 2023 Jan 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
Hadad E, Sualhi I, Legarda C, Seligman Y, Sorkin A, Dor O, Menashe S, Heller L, Wiser I. Silicone breast implant rupture is more prevalent in the dominant limb side: A retrospective cohort study. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2023 May;80:126-132. doi: 10.1016/j.bjps.2023.02.016.
Guimier E, Carson L, David B, Lambert JM, Heery E, Malcolm RK. Pharmacological Approaches for the Prevention of Breast Implant Capsular Contracture. Journal of Surgical Research. 2022 Dec;280:129-150. doi: 10.1016/j.jss.2022.06.073.
What Is Breast Implant Illness? Breastcancer.org.
Glicksman C, McGuire P, Kadin M, Lawrence M, Haws M, Newby J, Ferenz S, Sung J, Wixtrom R. Impact of Capsulectomy Type on Post-Explantation Systemic Symptom Improvement: Findings From the ASERF Systemic Symptoms in Women-Biospecimen Analysis Study: Part 1. Aesthet Surg J. 2022 Jun 20;42(7):809-819. doi: 10.1093/asj/sjab417.
Watad A, Rosenberg V, Tiosano S, Cohen Tervaert JW, Yavne Y, Shoenfeld Y, Shalev V, Chodick G, Amital H. Silicone breast implants and the risk of autoimmune/rheumatic disorders: a real-world analysis. Int J Epidemiol. 2018 Dec 1;47(6):1846-1854. doi: 10.1093/ije/dyy217.
Quinlan CS, Lynham R, Kelly JL. Risk Factor Analysis for Capsular Contracture, Malposition, and Late Seroma in Subjects Receiving Natrelle 410 Form-Stable Silicone Breast Implants. Plast Reconstr Surg. 2017 Sep;140(3):499e. doi: 10.1097/PRS.0000000000003613.
Calobrace MB, Stevens WG, Capizzi PJ, Cohen R, Godinez T, Beckstrand M. Risk Factor Analysis for Capsular Contracture: A 10-Year Sientra Study Using Round, Smooth, and Textured Implants for Breast Augmentation. Plast Reconstr Surg. 2018 Apr;141(4S Sientra Shaped and Round Cohesive Gel Implants):20S-28S. doi: 10.1097/PRS.0000000000004351.
Newman AN, Davison SP. Effect of Keller Funnel on the Rate of Capsular Contracture in Periareolar Breast Augmentation. Plast Reconstr Surg Glob Open. 2018 Jun 18;6(6):e1834. doi: 10.1097/GOX.0000000000001834.
Headon H, Kasem A, Mokbel K. Capsular Contracture after Breast Augmentation: An Update for Clinical Practice. Arch Plast Surg. 2015 Sep;42(5):532-43. doi: 10.5999/aps.2015.42.5.532.
Metzinger SE, Homsy C, Chun MJ, Metzinger RC. Breast Implant Illness: Treatment Using Total Capsulectomy and Implant Removal. Eplasty. 2022 Mar 16;22:e5.
Bird GR, Niessen FB. The effect of explantation on systemic disease symptoms and quality of life in patients with breast implant illness: a prospective cohort study. Sci Rep. 2022 Dec 6;12(1):21073. doi: 10.1038/s41598-022-25300-4.
Nagy, ES, Westaway, Mark, Danieletto, S, Afrin, LB. Breast Implant Illness May Be Rooted in Mast Cell Activation: A Case-Controlled Retrospective Analysis. Annals of Surgery 5(1):p e398, March 2024. | DOI: 10.1097/AS9.0000000000000398
Chen J, Zhu XM, Huynh MNQ, McRae M. Breastfeeding Outcome and Complications in Females With Breast Implants: A Systematic Review and Meta-Analysis. Aesthet Surg J. 2023 Jun 14;43(7):731-740. doi: 10.1093/asj/sjad027.
Stephen D Bresnick. Self-Reported Breast Implant Illness: The Contribution of Systemic Illnesses and Other Factors to Patient Symptoms. Aesthetic Surgery Journal Open Forum. Volume 5, 2023, ojad030. https://doi.org/10.1093/asjof/ojad030
The American Board of Cosmetic Surgery (ABCS) is the only certifying board that tests a surgeon’s knowledge and experience exclusively in cosmetic surgery. Our cosmetic surgeon Diplomates are carefully vetted for experience performing a full range of face, breast, and body cosmetic surgery procedures.